DataMatters - July 2023 Edition

In this Issue:
Publications and Data Releases
Opening Message
For the past few months CHIA staff has been working hard on several publications, which are expected to be released in coming months. Keep an eye out for the latest relative price data for Massachusetts hospitals and physician groups, a new health care equity report looking at hospital utilization by race and ethnicity, as well as a new report featuring readmissions data for the pediatric population in Massachusetts.
In June, CHIA held its second Oversight Council meeting of 2023. Oversight Council members discussed CHIA’s work on its new strategic plan, received an overview of priority analytic areas, as well as an update on the development of an enhanced All-Payer Claims Database (APCD) dataset. The Council meeting can be watched on CHIA’s YouTube channel here.
Don’t forget to also check our “Publications and Data Releases” section for a look at reports published since June, and “Upcoming Events and Resources” for notice of local events involving CHIA and/or related to health data.
We hope that you enjoy this newsletter, follow the links, and learn something new. If there’s something you enjoyed or if you have suggestions for improvement, we welcome your feedback at newsletter@chiamass.gov.
News You Can Use
Access to high quality primary care and behavioral health care has long been identified as essential to improving health outcomes and advancing health equity. Recent analysis by the Health Policy Commission (HPC) explored trends in these two service areas using CHIA’s primary care and behavioral health expenditure data and the Massachusetts All-Payer Claims Database (MA APCD). During their June commission meeting, the HPC walked commission members through findings from the forthcoming 2023 Health Care Cost Trends Report. The meeting recording is available on YouTube, and the presentation materials are available on the HPC’s website.
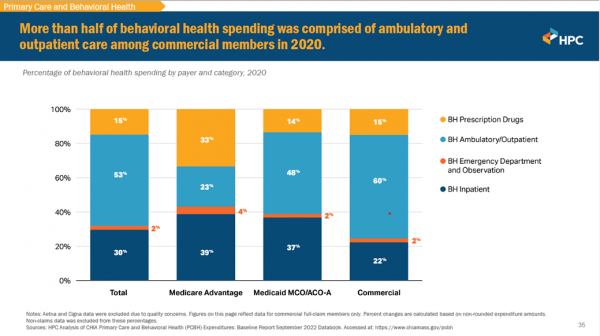
Examining the distribution of behavioral health care across inpatient and outpatient settings, the Health Policy Commission found that more than half of behavioral health spending was comprised of ambulatory and outpatient care among commercial members in 2020. In contrast, Medicaid and Medicare members had higher proportions of spending for inpatient care. This may be a reflection of the different types of care needed for these populations, a difference in the case-mix of these populations (e.g., MassHealth population may have a higher proportion of their population seeking BH care with serious mental illness), or a difference in access to outpatient services for these populations, and that additional research is needed to examine the drivers of these differences.
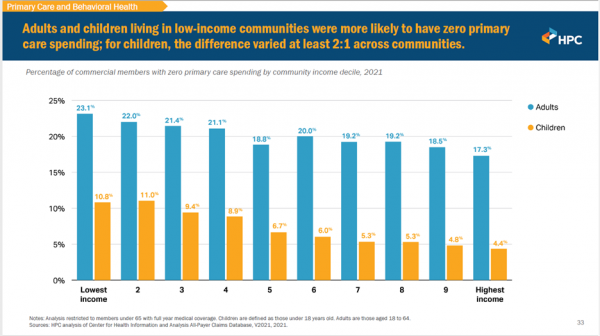
The Health Policy Commission also conducted an analysis of how primary care spending varies across Massachusetts communities. They found that residents living in lower-income communities were more likely to have zero primary care spending. This finding was even more pronounced for children living in low-income communities. In addition to identifying opportunities for improved primary care access in different parts of the Commonwealth, this research illustrates the importance of looking beyond aggregate results to compare how health care access and investment varies by sociodemographic characteristics and geography.
CHIA’s data is increasingly critical to understanding the Massachusetts health care landscape and helping to inform policymakers in health care decision making. Looking ahead, CHIA will be publishing updated primary care expenditure data early this fall, followed by a refresh of the primary care dashboard in early 2024.
The HPC is expected to bring the 2023 Health Care Cost Trends Report to the HPC Board for consideration at the public meeting on September 13, 2023.
Data User Profile
For each DataMatters newsletter, we feature an interview with a user of CHIA data. For this month, we reached out to one of the authors of an article published in the National Library of Medicine, BRCA1/2 testing among young women with breast cancer in Massachusetts, 2010-2013: An observational study using state cancer registry and All-Payer claims data.
Dr. Lydia Pace, Associate Professor at Harvard Medical School—along with her co-authors, John Z. Ayanian, Robert E Wolf, Richard Knowlton, Susan T. Gershman, Summer Sherburne Hawkins, and Nancy L. Keating—sought to understand whether there are racial/ethnic and socioeconomic disparities in breast cancer gene (BRCA) testing among young women with breast cancer in Massachusetts. For this study they utilized data from the Massachusetts All-Payer Claims Database (MA APCD).
We deeply appreciate Dr. Pace taking the time to answer our questions.
What was your research question? Why did you choose that question?
In this project we sought to examine how often young Massachusetts women with breast cancer (≤45 years) received guideline-concordant genetic testing after breast cancer diagnosis, and whether there were racial and ethnic or socioeconomic inequities in receipt of testing in our state in 2010-2013. We were particularly interested in understanding the extent to which inequities observed in other states exist in Massachusetts, a state with overall excellent access to care and where BRCA1/2 testing has been covered by both MassHealth and private insurance for some time.
Specifically, our research team is interested in care quality and equity in cancer screening, diagnosis and treatment. Because pathogenic variants in the BRCA1 and BRCA2 genes are strongly associated with early-onset breast cancer, the National Comprehensive Care Network in 2009 recommended that all women diagnosed with breast cancer at 45 or younger should be tested for BRCA1/2 pathogenic variants. Timely BRCA1/2 testing after a breast cancer diagnosis can inform individuals’ breast cancer treatment decisions as well as inform strategies to prevent other cancers. BRCA1/2 testing can also provide important information for individuals’ families. Despite the importance of BRCA1/2 testing for young individuals diagnosed with breast cancer, evidence from other states suggests that BRCA1/2 testing is not provided equitably, and that there are differences in indicated testing among different racial and ethnic and groups that vary by socioeconomic characteristics.
What CHIA data do you use?
We used the Massachusetts All-Payer Claims Data (APCD) from 2010-2014. Additionally, we used data from the Massachusetts Cancer Registry (MCR). Working with collaborators at MCR, we implemented a record linkage program developed by the Centers for Disease Control (called Link Plus) to link APCD enrollment data to MCR data. This linkage allowed us to build a cohort of individuals diagnosed with breast cancer and examine health services received before and after their cancer diagnosis. At the time of our study this type of linkage had not been commonly performed.
What was your experience using CHIA data?
The APCD data has unique value because it includes longitudinal data from both public (MassHealth) and private insurers throughout the state (although it does not include information on individuals working for large employers who are self-insured). Historically, such data have not been readily available to researchers. This permits examination of important policy questions, and studies can provide results that are more broadly generalizable than results from one insurer or one insurance type, and this made it particularly valuable for our analysis focused on inequities in care. Linking APCD with MCR data permitted us to leverage the strengths of each dataset to examine BRCA1/2 testing among what is likely a complete cohort of all young women diagnosed with breast cancer in MA during our study period. The linkage with MCR data was complex because CHIA data and MCR data are housed in different state agencies and both agencies have strict rules about sharing potentially identifiable data. Nevertheless, leaders in both agencies supported the project, and we were able to successfully perform the linkage.
Please briefly describe your research and key findings.
To assemble our study cohort, we identified breast cancer diagnoses in the Massachusetts Cancer Registry from 2010-2013. We matched patients in the registry data with patients in our Massachusetts APCD from 2010-2014. We included women aged ≤45 years with private insurance or Medicaid. We examined BRCA1/2 testing within 6 months of diagnosis and patient and clinician characteristics associated with testing.
In the cohort overall, 54.9% of individuals received guideline-concordant BRCA1/2 testing within 6 months of breast cancer diagnosis. However, in our logistic regression model, non-Hispanic Black women had less than half the odds of testing compared with non-Hispanic White women. MassHealth-insured women had half the odds of testing compared with privately insured women. Living in lower-income areas was also associated with lower odds of testing. Having an academically affiliated oncology clinician was not associated with testing.
Which findings were particularly interesting or surprising to you?
Our most notable findings were the inequities in testing rates. We found consistently lower BRCA 1/2 testing rates for Black women relative to White women in Massachusetts during our study period. We saw the same inequities for those insured by MassHealth compared with private insurance, and for those living in lower-income areas. We were surprised that individuals cared for by an academically affiliated oncology clinician were not more likely to receive guideline-concordant testing, though it would be valuable to examine other clinician and health facility characteristics in future work.
What "takeaway" information would you like to highlight from your research and/or experience using our data?
These findings are a reminder that even in a state that has prioritized health care access and insurance coverage, inequities in care quality and access to precision medicine persist and need intensive focus by clinicians, health systems and health policies. We hope that we can do a follow-up analysis to examine whether testing rates have improved with more attention to genetic testing and to precision medicine in general, and more awareness of BRCA1/2 pathogenic variants. It is also important to continue to investigate what provider and system factors can facilitate high-quality, equitable cancer care.
Publications and Data Releases
Quarterly Hospital Financial Performance through March 31, 2023
July 2023
CHIA earlier this month most recent quarterly acute hospital and health system financial performance report with data through March 31, 2023. Each quarter CHIA publishes this report on the profitability, liquidity, and solvency of hospital health systems and their affiliated acute hospitals, as well as the profitability of affiliated physician organizations.
HFY 2021 Hospital Health System Profiles
July 2023
CHIA also recently released Hospital Health System Profiles for FY 2021. Hospitals health system profiles provide a summary of financial performance and relative size of component entities for the hospital health system and their affiliated acute hospitals, physician organizations, and health plans. The profiles are accompanied by a technical appendix and individual system profiles.
Upcoming Events and Resources
Events and announcements of interest to our community, organized by CHIA, our data partners, and others
NAHDO 3rd Annual Meeting and In-Person Networking Session
August 14 – August 16, 2023
The National Association of Health Data Organizations (NAHDO) is hosting its annual meeting and a network workshop with topic-driven sessions designed to identify solutions to some of the current challenges facing health data organizations.
For more details and to register, click here.
The National Academy for State Health Policy (NASHP) 36th Annual Conference
August 14 – August 16, 2023
The National Academy for State Health Policy (NASHP) is hosting their annual conference in Boston this year. Join state leaders from around the country to discuss issues facing state health policymakers. More details to follow. Registration is open.
CHIA Data User Workgroups
Tuesday, August 22, 2023, 3:00 PM
These ongoing meetings are designed for data users and other interested parties to connect with CHIA to discuss analytical techniques and best practices in research using CHIA's MA APCD and Case Mix databases.
The next virtual workgroup meeting will be on Tuesday, August 22, 2023, at 3:00 PM. For more information including past presentations and user support materials, visit the information page. To learn more about CHIA data, please visit https://www.chiamass.gov/chia-data/.
Massachusetts Health Policy Commission
Board Meeting
Wednesday, September 13, 2023, 12:00 PM
The HPC’s 11-member Board meets approximately every six weeks throughout the year to review staff- (or guest)- presented overviews of the agency’s major workstreams, and other topics related to health care cost containment and reform. Major reports, statutory regulations, and publications are authorized by a majority vote at these meetings.
Betsy Lehman Center for Patient Safety
10th Annual Communication, Apology and Resolution (CARe) Forum
Friday, September 29, 2023, 9:00 AM – 1:00 PM
501 Boylston Street, 5th Floor, Boston, MA, 02116
This year’s Communication, Apology and Resolution (CARe) Forum will present case simulations and other material for live discussion in Boston, with an online option. Registration is free and open in early August. Visit BetsyLehmanCenterMA.gov/CARe for more information.
Massachusetts Association of Health Plans (MAHP) 2023 Annual Conference:
Health Care Affordability, Quality and Equity in a Post Pandemic World
SAVE THE DATE! Thursday, November 17, 2023, 7:30 AM – 2:00 PM
MA MAHP will be holding this year's conference at the Seaport Hotel on November 17th. Individual registrations will open in June. Please reach out to Ann Chamberlin at chamberlin@mahp.com to get information on available sponsorship opportunities.
Join Our Team
A selection of open positions at CHIA. Please feel free to share broadly with your network. Follow CHIA on LinkedIn for more regular updates.
Senior Health Care Data Liaison
Data Operations and Technology (DOT) Team
CENTER FOR HEALTH INFORMATION AND ANALYSIS
www.chiamass.gov
