DataMatters - November 2021 Edition
DATE: November 30, 2021

In this month’s DataMatters, we’re sharing an inside look at how CHIA data supports two critical Commonwealth missions: lowering health care costs and reducing administrative burden in regulation. In News You Can Use, you’ll learn more about recent analysis by the Massachusetts Health Policy Commission of CHIA’s Total Medical Expenses (TME) data, which is used as part of the state’s annual cost growth benchmarking process.
Our Data User Profile feature hands the pen to the Division of Insurance (DOI) for a description of how CHIA APCD data has helped free DOI and its regulated payers from participating in a quarterly data submission process payer-by-payer. As a one-stop data and technical assistance shop, CHIA is helping increase the Division’s speed and efficiency in achieving its mission to ensure the financial solvency of the companies it regulates.
Don’t forget to scroll to the end, where you’ll get to review the recent CHIA publications and data releases you might have missed, and a list of upcoming events that may pique your interest.
DataMatters is a newsletter for you, the stakeholders interested in the data we collect, release, and report on. We hope you will enjoy reading and learn something new, and we always want to know what you think. Please share your ideas and questions by emailing newsletter@chiamass.gov.
Our warmest wishes for a happy, and safe, holiday season. See you in 2022.
News You Can Use
Each year, as part of the Commonwealth’s health care cost growth benchmarking process, CHIA monitors the amount paid to providers for health care services delivered to a payer’s member population using a metric known as Total Medical Expense (TME). TME is also examined on a Health Status Adjusted (HSA) basis for each payer to reflect differences in member populations. CHIA reports on HSA TME in the agency’s Annual Report.
Recent analysis of unadjusted TME and HSA TME data by the Massachusetts Health Policy Commission (HPC) found meaningful differences trending the two metrics. Over a six-year period, HSA TME grew steadily at 7.6% (Figure 1). Disaggregating the components of HSA TME, the HPC found risk scores grew 15.0% at the same time. The rate of unadjusted growth in TME over this period was 22.6%. These differences have tangible implications for health policy decisions in Massachusetts.
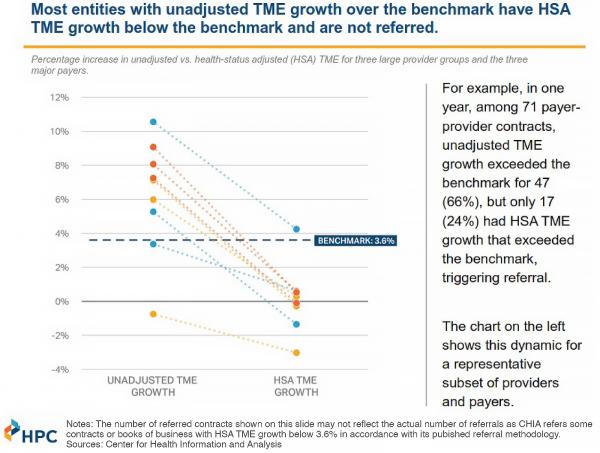
CHIA is statutorily responsible for confidentially referring a list of payers and primary care providers whose increase in HSA TME jeopardizes the state’s ability to meet the health care cost growth benchmark to the HPC every year. In an effort to understand how those referrals may be impacted by this trend, the HPC also compared unadjusted and HSA TME for three large provider groups and the three major payers. Among the sample of 71 payer-provider contracts that were examined, unadjusted TME growth exceeded the benchmark for 47 (66%), but only 17 (24%) had HSA TME growth that exceeded the benchmark, triggering referral (Figure 2).
These findings have led the HPC to recommend that the Legislature allow CHIA to use additional metrics besides HSA TME to determine whether a provider or payer should be identified as contributing to excessive health care spending.
CHIA will continue to report on spending trends in its Annual Report. Tune in late winter ’22.
Figure 1
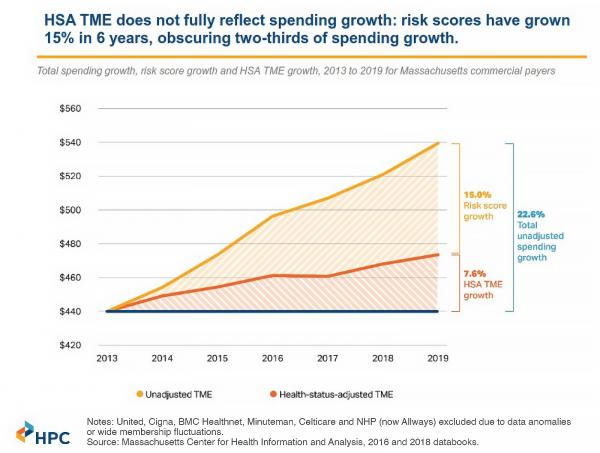
Figure 2
Data User Profile
Each edition of DataMatters features an interview with a CHIA data user, focusing on their experience obtaining and using our data and how it is used. We are grateful to Kevin Beagan, Deputy Commissioner at the Massachusetts Division of Insurance (DOI), for his interest in discussing the DOI’s ongoing use of CHIA APCD data as the basis for its quarterly HMO Membership Reports (and in the future, adding Utilization Reports).
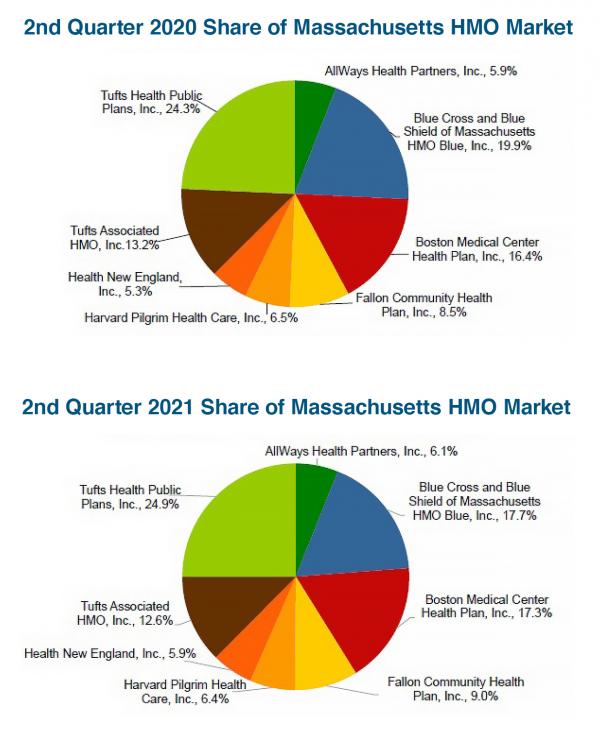
These second quarter HMO Membership Reports, produced by the Massachusetts Division of Insurance using CHIA’s APCD data and technical assistance, shows shifting payer market shares in fully-insured HMO products over the past few years (shown above: 2020 and 2021).
Which CHIA data did you use?
Member Eligibility and Product files from a select group of payers. The process runs directly against CHIA’s APCD Data Warehouse to produce the reports.
Why APCD data?
The Division of Insurance relies upon regular membership and utilization reports from licensed health carriers [focusing on HMO carriers] to track changes in individual company operations and overall market trends. While we [previously] collected this information from carriers, in order to promote administrative simplification, we have worked with carriers and CHIA to develop summary reports from the APCD so that companies do not need to submit information to the Division.
Why is the reporting limited to HMOs?
Insurance companies usually offer a number of products. For example, United Healthcare can offer dental, vision or disability income products under its license. HMOs are restricted to offering comprehensive health products and we track their business in particular because coverage can be volatile with changes in the market, and this could markedly impact the financial health of any one HMO company. Only fully-insured (aka not self-insured) HMO business is tracked. Note: DOI’s primary mission is to monitor the solvency of its licensees in order to promote a healthy, responsive and willing marketplace for consumers who purchase insurance products.
Please describe your experience using CHIA data?
CHIA staff have been extremely supportive throughout our process to assist with creation of appropriate computer coding needed to aggregate and develop reports. They have also helped to develop a process for carriers to validate the reasonableness of the information generated from the APCD. While we have been able to establish a regular process for APCD-generated membership reports, utilization is trickier and we are still going through a vetting process with carriers to make sure that the codes being used to group data are properly reporting carrier utilization. We hope to be producing regular utilization reports starting in 2022.
Which type of APCD data (e.g., data fields or calculations) is critical to your reporting?
Membership, as well as inpatient, outpatient, and pharmacy claims data.
What takeaway information would you like to highlight from your experience using our data?
It is necessary to have a feedback loop with carriers to validate that the reported information is consistent with their own experience. It is important to do careful work upfront to make sure that computer logic will pick up any unique characteristics of a company’s APCD data and that companies are able to see the APCD-reports so that they can validate that the information is correct and/or suggest changes that may need to be made to their APCD data.
Publications and Data Releases
CHIA released its review of An Act relative to mental health providers (H1114/S1262) to the legislature and online last week. CHIA is statutorily required to produce these reviews, which assess proposed new insurance mandates for potential efficacy and likely impact of the mandate on health costs (via fully-insured health plans). The bills in question would require occupational therapists (OTs) and occupational therapist assistants (OTAs) to be statutorily recognized as mental health providers and therefore require health plans to reimburse for their provision of mental health services.
The latest quarterly update to the Massachusetts Acute Care Hospital Inpatient Discharge Data (FFY 2016-2019) report was released last month. It includes data from October 2018 – June 2021. Using interim data, the update offers insights into patterns and trends on key inpatient utilization measures through a series of interactive dashboards; also included are the report overview, technical appendix, and Excel databook.
Upcoming Events and Resources
Events and announcements of interest to our community, organized by CHIA, other Commonwealth agencies, and others.
CHIA’s Oversight Council meets quarterly to discuss agency updates and priorities. The next meeting is scheduled for Monday, December 6 and will be live streamed on CHIA’s YouTube channel.
The MMS, a statewide professional association for physicians and medical students, will host its Annual Oration in December. The 2021 Annual Oration will reflect and explore the mindset and skills essential to effective leadership before, during and after a public health crisis. Dr. Monica Bharel–Commissioner of the Massachusetts Department of Public Health from 2015-2021–will share her experience leading through crises, including the COVID-19 pandemic, and how it can help better inform our work to respond to future crises more effectively and equitably. The talk will take place December 2 at 7 p.m. on Zoom. Registration is required. Tickets cost $80 for non-member professionals.
CHIA is an affiliate member of the Massachusetts Health Data Consortium, a trade association focused on connecting members of the Commonwealth’s health care community in their use of data, analysis, and information technology to achieve sustainable improvements in quality, cost, and effectiveness.” The association sponsors regular webinars and podcasts focusing on health data and policy-related issues, including several in the coming months.
The Health Policy Commission has posted its 2022 Public Meeting Calendar. Remaining public meetings for 2021 are: Advisory Council - December 8 at 12 p.m., and monthly Board Meeting – December 14 at 12 p.m. Meetings are held virtually and broadcast live on the HPC's YouTube channel.
The Massachusetts Health Connector is the state's Marketplace for health and dental insurance. Health Connector plans are open to Massachusetts individuals and families who do not have access to affordable coverage through a job, and financial assistance is available to those who qualify. The Health Connector’s Open Enrollment period for 2022 coverage is now open, and will run through January 23rd. Residents looking for coverage that begins on January 1st need to pick a plan and make a payment by December 23rd. Thanks to the American Rescue Plan, the COVID-19 stimulus bill passed in March, more assistance lowering premiums is available to more people than ever before. Visit www.MAhealthconnector.org to learn more about plan options, help lowering costs, and to fill out an application.
CENTER FOR HEALTH INFORMATION AND ANALYSIS
www.chiamass.gov
