DataMatters - September 2021 Edition
DATE: September 30, 2021

Health care quality is the focus of September’s DataMatters. We proudly announce the release of our latest Quality of Care in the Commonwealth dashboard, profiled in this issue’s “News You Can Use” section. Continuing on this theme, the “Data User Profile” section highlights a recent external study that used CHIA’s MA-APCD data to show what happened to health costs and utilization when one widely-used quality measure – outpatient follow-up within 30 days after an emergency department visit for mental illness – is put into practice.
CHIA is also partnering with the Massachusetts Health and Hospital Association and select acute care hospitals to pilot a program to reduce readmissions and enhance patient experience. To support this effort, CHIA shared data from its enhanced analysis of all-payer, unplanned readmissions, which incorporates community-level social risk factors with the hospitals. The goal of this program is to help hospitals better understand how patient and community social risks factors may impact their hospital readmissions rates and how they may better target their efforts to reduce readmissions and enhance patient experience. Hospitals’ feedback will be incorporated into CHIA’s next annual readmissions report, due out later this year.
Don’t forget to check our “Publications and Data Releases” section for a retrospective view of reports published since Aug. 1, and “Upcoming Events and Resources” for notice of local events involving CHIA and/or health data.
We hope you’ll enjoy this newsletter, follow the links, and learn something new. If there’s something you enjoyed or if you have suggestions for improvement, we welcome your feedback at newsletter@chiamass.gov.
News You Can Use
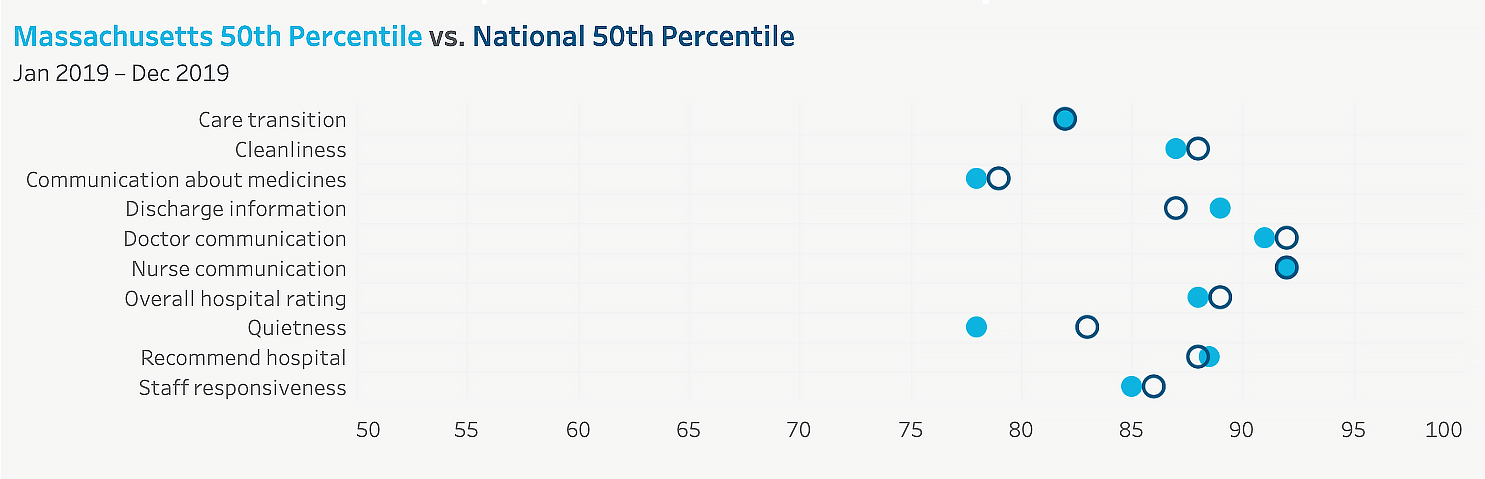
CHIA is pleased to announce the release of the latest Quality of Care in the Commonwealth interactive dashboard, with accompanying data and technical appendix. The dashboard covers health care quality measures gathered from multiple data sources and reported both at the statewide level, as in the example shown below, and for individual Massachusetts providers.
In 2019, Massachusetts’ 50th percentile hospital patient experience scores for measures of patient satisfaction with the discharge information they received, and willingness to recommend the hospital, exceeded the same scores on a national level
This year’s dashboard includes information on Healthcare-Associated Infections, Medication Safety, Mortality, Maternity, Effective Care Processes, and Patient Experience at individual Massachusetts hospitals, health systems (larger entities including multiple hospitals and providers), and medical/physician groups. It is an update to the May 2019 “CHIA Focus on Provider Quality Interactive Data.”
This refresh only includes quality data through 2019. Quality measure reporting was, in many cases, put on hold while the health care system responded to the pandemic, so 2020 data was either not collected, or providers were able to submit 2019 scores to meet reporting requirements in order to avoid unfair penalties. CHIA looks forward to updating with available data from during and/or following the pandemic response in our next refresh.
Data User Profile
Each edition of DataMatters features an interview with a recent user of CHIA data, focusing on their experience obtaining and using the data in addition to research outcomes. We are grateful to Dr. Kimberly H. Geissler of University of Massachusetts Amherst, for her interest in discussing her (and her co-authors, Michael Cooper and John Zeber)’s use of CHIA APCD data as the basis of the July 2021 Administration and Policy and Mental Health article, Association of Follow-up after an Emergency Department Visit for Mental Health with Utilization Based Outcomes .

What was your research question? Why did you choose that question?
We were interested in whether outpatient follow-up within 30 days after an emergency department visit for mental illness was associated with costs and utilization outcomes. We chose this question because although this follow-up metric is a new and widely used quality measure, there is little empirical evidence on whether follow-up improves future outcomes. As more than 4% of ED visits have a mental health condition or substance use disorder as the primary diagnosis, with increasing rates over time, understanding implications of timely follow-up care is warranted.
Which CHIA data did you use?
We used the APCD version 5.0, including 2011-2015. We primarily used the Medical Eligibility and Medical Claims data.
What was your experience using CHIA data?
I have used APCD data extensively since 2013, soon after it became available. I greatly appreciate the comprehensiveness of the data at the state level. One feature of the APCD that was particularly important for this research was the ability to analyze people who had either commercial or Medicaid insurance. With each version of the data, CHIA has made it easier for researchers to apply for and analyze, which I appreciate. Our work was funded by the National Institute for Health Care Management.
Please briefly describe your research and key findings:
Using APCD data, we identified individuals who had an emergency department (ED) visit for mental illness, and then followed them over time to determine if they had follow-up within 30 days and their health care use in the following six months. We then analyzed the association of having follow-up with costs and acute care utilization in the six months following the ED visit. We found that only one-third of patients had a follow-up visit for mental illness within 30 days. Adjusted regression analyses show timely follow-up is associated with significantly increased costs, an increased probability of inpatient hospitalization, and a small reduction in the probability of at least one additional ED visit.
Which findings were especially interesting, or surprising for you?
We were surprised by the low rates of follow-up in this population, and by the fact that the results did not substantively differ when we controlled for previous connection to the health care system. Better understanding influences of hospital and outpatient delivery system characteristics on achieving follow-up within the appropriate time period will be of importance in translating these findings into clinical practice.
What "takeaway" information would you like to highlight?
The CHIA APCD data is a unique and powerful resource for researchers to understand the healthcare system in Massachusetts. The available inclusion of Medicaid data is an important distinction from other datasets covering the commercially insured and allows for very detailed analyses of vulnerable populations.
Publications
Today CHIA published the latest Acute Hospital and Health System Financial Performance report, including data from acute hospitals, associated health systems, and physician organizations for the period ending June 30, 2021. The period ending June 30, 2020, which is used as a comparison for the data in this report, includes the first few months of the impact of COVID-19 on health care operations. COVID-19 relief funding was distributed beginning in April 2020 and a portion of this funding was reported as operating revenue.
September 2021
CHIA’s Massachusetts Hospital & Health System Financial Performance, FY2020 report, including a five-year retrospective trend analysis, was released on Sept. 23. The report examines the profitability, liquidity, and solvency of Massachusetts hospital health systems and their affiliated acute hospitals, and profitability of their affiliated physician organizations and health plans. It includes F2020 data, thereby incorporating the financial impact of COVID-19 on hospitals (including federal and state COVID-19 relief funding that hospitals received).
Upcoming Events and Resources
This section includes events and announcements of interest to our community, organized by CHIA, other Commonwealth agencies, and others.
HLTH 2021 is the preeminent event designed for the health industry, bringing together senior leaders to solve healthcare’s most pressing problems and realize the most promising opportunities to create health’s future. HLTH features four days of inspiring content, curated networking, educational sessions, and dynamic events for payers, providers, employers, investors, startups, life sciences, policymakers and innovation centers. The conference is co-sponsored by Mass Digital Health, a comprehensive public-private partnership working to establish Massachusetts as a leading ecosystem for digital health innovation, driving economic impact and improving healthcare costs and quality.
The Massachusetts Health Policy Commission (HPC) hosts an Annual Health Care Cost Trends Hearing each fall. The hearing is a public event at which elected officials, policymakers, researchers, and health care market participants convene to address challenges and discuss opportunities for improving care and reducing costs in the Commonwealth, the state’s performance under the Health Care Cost Growth Benchmark, drivers of health care costs, and other health care reform efforts. The HPC also released its 2021 Cost Trends Report earlier this month. This year’s hearing will air on a virtual platform between noon - 4 p.m. Register for an invitation to watch live.
CHIA’s appointed Oversight Council meets quarterly to discuss agency priorities and agenda-setting. The next meeting is scheduled for Monday, December 6 and will be aired live on CHIA’s YouTube channel.
The Massachusetts Health Connector is the state's Marketplace for health and dental insurance. Health Connector plans are open to Massachusetts individuals and families who do not have access to affordable coverage through a job, and financial assistance is available to those who qualify. Thanks to the American Rescue Plan, the COVID-19 stimulus bill passed in March, additional assistance is now available, including low- and no-cost plans to those currently receiving unemployment benefits. Click to learn more about this new benefit, or review the FAQ or this video produced by the Massachusetts Health Connector. You can also apply for or update a Health Connector account at www.MAhealthconnector.org to see if you qualify. When you apply, include information about your unemployment benefits so the Health Connector can check to see if you qualify.
CENTER FOR HEALTH INFORMATION AND ANALYSIS
www.chiamass.gov