DataMatters - July 2021 Edition
DATE: July 30, 2021

If you’re not lucky enough to be on vacation right now, may you find temporary repose catching up with CHIA’s recent reports and data asset updates in this issue of DataMatters. This month’s issue features the latest snapshots of our data users. See “News You Can Use” to learn about the agency’s first report documenting unmet health-related social needs using the Massachusetts Health Insurance Survey, or our “Data User Profile,” which features a Texas-based research team that used CHIA's hospital discharge data to inform their just-published study, Emergency Department Utilization by Adolescents Experiencing Homelessness in Massachusetts. CHIA also recently published reviews of mandated health insurance benefits in the Commonwealth, hospital and health system financial data, and an examination of provider price variation using Relative Price.
DataMatters is a newsletter for you – all stakeholders interested in the data we collect, release, and report on. We hope you will enjoy reading and learn something new. We also want to hear your opinions on what you’ve read and what you’d like to see in our next issue. Please let us know by emailing newsletter@chiamass.gov.
News You Can Use
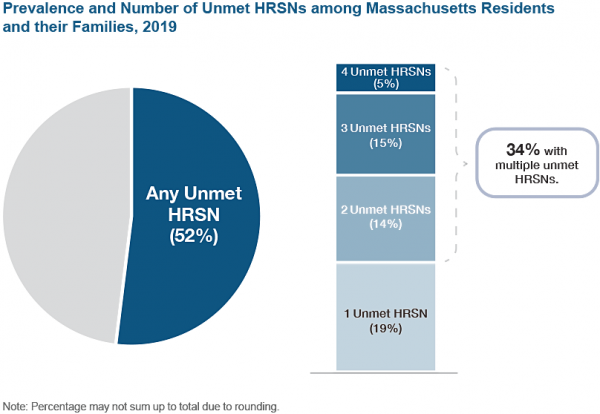
CHIA expanded the scope of reporting from its Massachusetts Health Insurance Survey (MHIS) last month to include a new area of study – Social Determinants of Health – with the research brief Over Half of Massachusetts Residents Report Unmet Health-Related Social Needs in Their Families. The MHIS is a Massachusetts household survey fielded every other year. The Unmet Health-Related Social Needs (HRSN) research brief documents the prevalence of unmet HSRNs in Massachusetts. Residents who reported food insecurity, housing instability, financial strain, or employment instability in their families were considered to have an unmet HRSN. The research brief found that the majority (52%) of all Massachusetts residents reported at least one unmet HRSN in their families in 2019, and over one-third (34%) reported multiple unmet HRSNs. Unmet HRSNs were experienced by residents and their families at all income levels, across race/ethnicity groups, and across all family types. However, residents with very low or low income, residents of color, and residents in single-parent families experienced unmet HRSNs at significantly higher rates than their counterparts. The full brief contains more details on the findings. It is CHIA’s first step to document the burden of unmet HRSNs in Massachusetts and better understand how they are experienced by residents and their families across the state.
Data User Profile
What was your research question? Why did you choose that question?
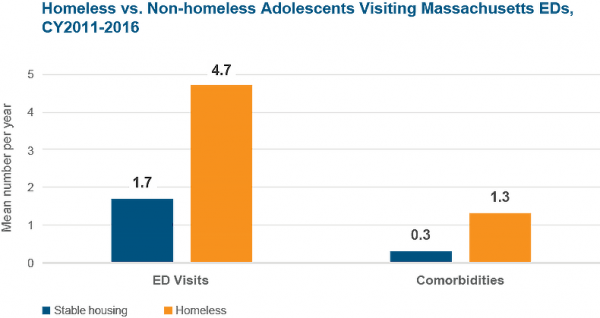
TG: Our questions were: 1) How many times more do homeless adolescents go to the Emergency Department (ED)? 2) Of those who go to the ED, what characteristics drive them there? We had been working with HCUP data for different projects, but once we got our hands on Massachusetts data, we saw that there was a homeless indicator. The homeless indicator gives researchers leverage to do novel work, present new findings and help policymakers.
HK: In my experience there are not a lot of databases that track homeless people. We were able to cross-check the indicator with ICD-9 codes and by checking with hospitals. We decided to go ahead with the paper after talking to the hospitals.
Which CHIA data did you use?
TG: We got our data, covering 2011-2016, through HCUP [DataMatters note: CHIA periodically submits Case Mix Emergency Department and Hospital Inpatient Discharge data collected from Massachusetts hospitals to HCUP].
What was your experience using CHIA data?
TG: It was pretty simple to get. You just write up a page describing your research project, apply, and HCUP makes a decision within two to six weeks. You can buy individual states, or national samples.
HK: Massachusetts is one of the few databases to have a homeless indicator. We also liked that each patient has a unique hashed (masked) identifier; you can follow and track the patients across providers and years.
Please briefly describe your research and key findings:
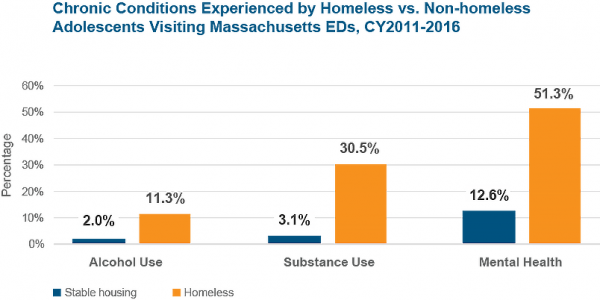
TG: The 10,000 homeless adolescents in our study accounted for 46,000 ED visits – about five visits per year, which was disproportionately high compared to non-homeless cohort. Another big finding at this point was that mental health and substance use disorders were really, really high for homeless adolescents compared to a non-homeless comparison group.
Which findings were especially interesting, or surprising for you?
TG: Homelessness is associated with more ED visits - the takeaway is that housing seems to be and is a separate social determinant of health. Also, we realized that more than 50% of the homeless cohort of adolescents tracked were on Medicaid.
What "takeaway" information would you like to highlight?
TG: Three main messages: 1) Housing is a separate social determinant of health; 2) The importance of having the homeless indicator in large secondary databases; 3) Providers should have assistance on-hand to refer homeless adolescents to services addressing food insecurity and housing insecurity, once they leave the ED. Also, providers should have support and training to promote non-judgmental care that these individuals need.
HK: When a homeless teen visits an ED for the first time then you can try to meet their social needs and avoid future ED visits.
Publications
Summer 2021
CHIA recently released hospital inpatient and emergency department discharge data (Case Mix) for FY20. Case Mix is one of CHIA’s most-requested data assets and the one that has been in production the longest. The data is also shared with the Healthcare Cost and Utilization Project (HCUP), the U.S. government national hospital discharge dataset used by researchers nationwide.
Upcoming Events and Resources
CHIA’s activities are guided by an 11-member Oversight Council with a wide range of experience and expertise in health care, technology, and related fields. The Oversight Council meets quarterly and meetings are live streamed and available as recordings on CHIA’s YouTube channel. An agenda for September’s meeting is forthcoming.
Staff from CHIA’s Strategies and Research Team will be presenting at the National Association of Health Data Organizations’ (NAHDO) 36th Annual conference, to be held virtually.
- Timeliness and Accessibility: Developing an Interactive Dashboard for Quarterly Updates on the Massachusetts Acute Care Hospital Inpatient Discharge Data. (Part of Spotlight Series presentations, time TBD)
- A Methodology to Identify and Analyze Hospitalizations with Behavioral Health Comorbidities: Preliminary Findings from the COVID-19 Pandemic (Session Title: Health Databases and COVID-19: Adapting the Data, Responding to Trends; Sept. 28, 3:20 p.m.)
- How does COVID-19 Impact Statewide Readmission Trends in Massachusetts? (Session Title: Adopting Methodologies to Better Track COVID-19 and other novel phenomena, Sept. 30, 12:50 p.m.)
Massachusetts Health Connector Low- or No-Cost Premiums available to Unemployed
The Massachusetts Health Connector is the state's Marketplace for health and dental insurance. Health Connector plans are open to Massachusetts individuals and families who do not have access to affordable coverage through a job, and financial assistance is available to those who qualify. Thanks to the American Rescue Plan, the COVID-19 stimulus bill passed in March, additional assistance is now available, including low- and no-cost plans to those currently receiving unemployment benefits. Click to learn more about this new benefit, or review the FAQ or this video produced by the Massachusetts Health Connector. You can also apply for or update a Health Connector account at www.MAhealthconnector.org to see if you qualify. When you apply, include information about your unemployment benefits so the Health Connector can check to see if you qualify.
CENTER FOR HEALTH INFORMATION AND ANALYSIS
www.chiamass.gov
