DataMatters - January 2022 Edition

In this Issue:
Publications and Data Releases
Opening Message
Happy 2022! With this publication, DataMatters marks one year of bringing CHIA data, its uses, and end-user products to your inboxes. We're pleased to celebrate this milestone with you, and hope you find inspiration in what we've highlighted.
In this edition, we take on the hot topic of health equity. CHIA's newly-published Health Insurance Coverage and Care in Massachusetts, 2015-2019: A Baseline Assessment of Gaps by Age, Race and Ethnicity, and Income, profiled in the "News You Can Use " section below, focuses on several factors as measured by the agency's Massachusetts Health Insurance Survey in the period leading up to the COVID-19 pandemic. Physical ability (or disability) status can also determine whether two people receive the same health care – as documented by findings from a University of Michigan-Brandeis University team whose September 2021 research is featured in our "Data User Profile." The team used CHIA's All-Payer Claims Database (APCD) to explore whether deaf or hard-of-hearing individuals received comparable contraceptive care during a study period. They discussed their findings and experiences using our data with DataMatters. More data is just around the corner, with CHIA's Annual Report on the Performance of the Massachusetts Health Care System and its analysis of total health care expenditures in Massachusetts set for release in March, when it will be discussed at the Massachusetts Health Policy Commission's annual Cost Growth Benchmark hearing, scheduled for March 16, as you'll see in our Calendar section.
We hope you will enjoy reading this one-year anniversary edition of DataMatters. We'd love to hear what you think! Please write to us anytime, at newsletter@chiamass.gov.
News You Can Use
Showcasing CHIA researchers’ use of our data
This issue’s “News You Can Use” focuses on CHIA’s new research series focusing on health care equity issues in the Commonwealth. The first installment, Health Insurance Coverage and Care in Massachusetts, 2015-2019: A Baseline Assessment of Gaps by Age, Race and Ethnicity, and Income, was released in December. It documents health insurance coverage, access, utilization, and affordability during the period leading up to the COVID-19 pandemic.
Broadly, CHIA found that Massachusetts residents’ ability to access, use, and afford health care differed by population subgroups. Findings of particular interest to the team included:
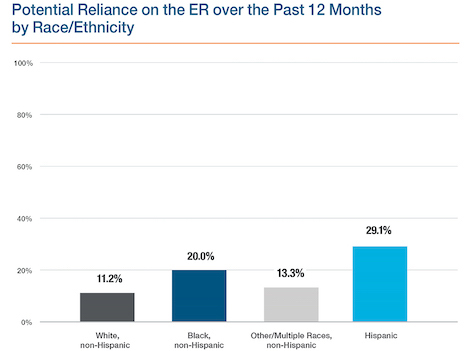
- Compared to White residents, Black residents were nearly twice as likely to have a potential reliance on the ER for care. Hispanic residents were nearly three times as likely.
- The racial/ethnic differences in access to health care were most prominent among residents with moderate family income: 39.3% of Hispanic residents reported difficulties accessing care at a doctor’s office or clinic, compared with 29.6% of White residents.
- Within every racial/ethnic group, the highest rates of family medical debt or problems paying family medical bills were for residents in the moderate family income group.
The COVID-19 pandemic has brought renewed attention to the health care disparities that are present in Massachusetts despite the state’s high health insurance coverage rate and strong access to and use of health care. These findings highlight the fact that people continue to struggle with areas of access, use, and affordability.
The second part in the Health Equity series, planned for release in the spring, will focus on the impact of differences in geographic regions across Massachusetts.
Data User Profile
Each edition of DataMatters features an interview with an external CHIA data user, focusing on their experience obtaining and using our data and how they used it. We are grateful to Dr. Justine Wu, of the University of Michigan, and her colleagues (at Brandeis University and U-MI) who used CHIA APCD data as the basis for their September 2021 research, Contraceptive Provision and Quality Care Measures for Insured Individuals in Massachusetts Who Are Deaf or Hard of Hearing, for talking with us about the research.
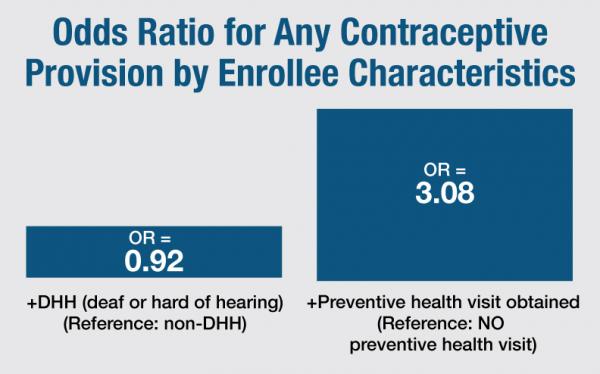
CHIA-produced graphic using authors’ data calculations. Graphic depicts odds ratio of Massachusetts commercially-insured enrollees in 2013-2014 receiving contraception, depending on whether they were deaf or hard of hearing (left bar) or whether they obtained a preventive health visit (right bar). Source: MA APCD
What was your research question? Why did you choose that question?
We sought to use claims data analysis to describe contraceptive provision for insured individuals in Massachusetts who are deaf or hard of hearing (DHH), and compare to provision for those who are not deaf or hard of hearing (non-DHH). DHH individuals face significant structural challenges to accessing equitable health care services, such as the lack of equipment and personnel (e.g., ALS interpreters) to facilitate patient-provider communication during clinical encounters. Hearing loss alone does not pose any restrictions on the type of contraception one can use, and studies have indicated that the level of sexual activity is similar between DHH and non-DHH individuals. Thus, DHH individuals should theoretically have similar patterns of contraceptive use as their non-DHH counterparts.
Which CHIA data did you use?
2013-2014 Medical Claims, Pharmacy Claims and Eligibility files.
What was your experience using CHIA data?
Our team has used CHIA data in the past for other studies, including an analysis to determine contraceptive provision for individuals with intellectual and developmental disabilities. The Pharmacy Claims data field showing NDC (National Drug Code) is particularly helpful to use to ascertain contraceptive prescriptions and insertion of contraceptive devices. One limitation of insurance claims data is that it is hard to determine the number of enrollees who rely upon tubal sterilization or vasectomy of their partner for contraception. This limitation stems from the fact that sterilization surgeries generate a procedure code only once and will not be captured in years subsequent to the surgery. Thus, we can estimate the annual prevalence of sterilization, but not the cumulative prevalence of sterilization over time.
Please briefly describe your research and key findings
- We identified 1,171,838 enrollees at risk for pregnancy; 1.1% (13,400) had a diagnosis for deaf or hard of hearing.
- Among DHH individuals, 29.7% were provided contraception during the index year of analysis. DHH individuals were slightly less likely to receive prescription contraception than non-DHH individuals (8% lower odds).
- A slightly greater percentage of DHH individuals received no contraceptive prescriptions or services (e.g., IUD placement, sterilization) compared to non-DHH individuals (70.4% versus 68.6%, p<0.01).
- There were no differences in provision of the most effective methods (IUDs, implant, sterilization) by deaf and hard-of-hearing status.
- DHH enrollees and non-DHH enrollees were similar with respect to attending a preventive health visit (68% vs. 61% respectively, a non-significant difference).
- Among all enrollees, regardless of DHH status, receipt of a preventive health visit was strongly associated with receipt of contraception (Odds ratio 3.0)
Which findings were particularly interesting, or surprising for you?
We identified disparities in contraceptive provision for DHH individuals, which were smaller than we expected. This is a promising finding, but must be considered in context of state-level health policy.
6. What "takeaway" information would you like to highlight from your research and/or your experience using our data?
Overall, we found modest evidence that insured DHH individuals in MA were less likely to receive prescription contraception than their non-DHH counterparts. We also found a strong association between contraceptive provision and receipt of a preventive health visit, regardless of DHH status. This finding, coupled with the high prevalence of preventive health visit attendance by DHH individuals (68%), suggests that insurance coverage for contraception and preventive health services are critical to access to contraception for this population. Our findings may be unique to Massachusetts because of its decades of experience with health care reform and near universal insurance coverage for its residents including contraceptive prescriptions and devices without cost-sharing. They may not be generalizable to states with lower levels of insurance coverage and more restrictive contraceptive policies.
Publications and Data Releases
CHIA released the latest update to the All-Payer Claims Database (MA APCD) dataset in December. It includes Massachusetts health claims data from the initial months of COVID-19 (the total dates included are January 1, 2016 – December 31, 2020, as paid through June 30, 2021). Data was collected from private and public insurers who pay eligible health care claims for Massachusetts residents; and eight file types, including medical, pharmacy, and dental claims with associated membership, provider, product, and benefit plan data. CHIA and external researchers use APCD data to inform published articles and reports about health costs and access; for a sampling of work by external researchers, visit CHIA’s recently updated Resultant Research page.
Last week, CHIA released the first statewide report on utilization and trends in hospital outpatient observation visits in the Commonwealth. Massachusetts Acute Care Hospital Outpatient Observation Data (FFY 2016-2019) presents key measures of outpatient observation care utilization overall and by hospital, patient demographic, and visit characteristics in the period leading up to the outbreak of COVID-19. Outpatient observation visits are classified as a type of outpatient care that can include assessment of patients who may require additional treatment beyond care in the emergency department, but not admission to the inpatient setting. Key findings from the new report include: In FFY 2019, there were 330,324 total observation visits among Massachusetts acute care hospitals, one-third of which resulted in an inpatient admission; and the most common expected primary payer type for observation visits was Medicare (42.4%), followed by commercial insurance (27.6%) and Medicaid (22.7%).
Also in December, CHIA released a first-of-its-kind report on health care equity in Massachusetts: Health Insurance Coverage and Care in Massachusetts, 2015-2019: A Baseline Assessment of Gaps by Age, Race and Ethnicity, and Income. It provides a baseline assessment of gaps in health insurance coverage, access, utilization, and affordability in the period leading up to the COVID-19 pandemic based on the above characteristics; findings document disparities in continuous health insurance coverage, access to care, and medical debt load by both racial/ethnic group and income. Special Note: Be sure to watch our two-minute video interpretation of report highlights.
The most recent edition of CHIA’s quarterly update to the Massachusetts Acute Care Hospital Inpatient Discharge Data (FFY 2016-2019) report, released in December, covers key inpatient utilization patterns and trends (including COVID-19) via a series of interactive dashboards. The current edition includes data from October 2018 -September 2021.
The most recent edition of this report was released in late December. It provides a quarterly update on profitability, liquidity, and solvency for the fiscal year-to-date period ending September 30, 2021. Note, since most hospitals and health systems have a September 30th fiscal year end, data for those hospitals were not yet due at the time of publication and will be released at a later date.
In November, CHIA released its review of An Act relative to mental health providers (H1114/S1262) to the legislature; it is also posted on CHIA’s website. CHIA is statutorily required to produce these reviews, which assess proposed new insurance mandates for potential efficacy and likely impact of the mandate on health costs (via fully-insured health plans). The proposed bill would require occupational therapists (OTs) and occupational therapist assistants (OTAs) to be statutorily recognized as mental health providers and therefore require health plans to reimburse for their provision of mental health services.
Last week, CHIA also released an update to the Comprehensive Mandated Benefit Review which was originally published in July 2021. The updated review includes required direct cost (RDC) calculations for the 45 health insurance mandates in effect as of 2018. RDC represents the costs of all services described in the mandates, as well as corresponding administrative costs, paid for by the regulated insurance plans, whether or not the costs would have been incurred in the absence of the mandate through voluntary provision of the benefits. The review had previously solely focused on measuring the marginal direct costs of the mandates, or costs above and beyond those that would be present even if the mandate law were not in force.
Upcoming Events and Resources
Events and announcements of interest to our community, organized by CHIA, other Commonwealth agencies, and others.
CHIA hosts monthly, public workgroups as opportunities for external users of the APCD and Case Mix databases to meet with CHIA’s in-house data experts to discuss analytical techniques and data questions. CHIA staff answer pre-submitted questions about the data and announce news of data releases and enhancements. Meetings alternate between APCD and Case Mix; the next workgroup, focusing on Case Mix data, will be hosted on Zoom on Feb. 15 at 3 p.m. For more information or to register, visit the information page.
CHIA Oversight Council
Next: March 22
CHIA’s appointed Oversight Council meets quarterly to discuss agency priorities and agenda-setting. The next meeting is scheduled for Tuesday, March 22, at 11:30 a.m. and will stream live on CHIA’s YouTube channel.
The Massachusetts Health Policy Commission will host its annual Cost Growth Benchmark Hearing on Wednesday, March 16 (12:00 – 3:00 pm); meeting will be aired live on the HPC’s YouTube channel. Under state law, the HPC Board sets the benchmark – which is a goal that total health care spending by all payers in the state will not grow faster than the state’s economy - each calendar year annually between January 15 (when the potential gross state product is established) and April 15. The process relies on data reported in CHIA’s Annual Report on the Performance of the Massachusetts Health Care System. More information about the benchmark modification process and details about the upcoming hearing are available on the HPC’s website.
The coronavirus pandemic has left health care workers mentally fatigued, causing many to leave the industry. STAT News hosts this free, virtual event to discuss ways to support and retain clinicians and other staff. Register here. See more upcoming STAT News events here.
The MHA is co-producing a series of webinars that encourage dialogue and share best practices. The next in the series will feature Juan Fernando Lopera, Chief Diversity, Equity, and Inclusion Officer at Beth Israel Lahey Health, speaking on “Building the Business Case” for diversity, equity, and inclusion in the workplace. For more information and to register, visit (here).
The APCD Council is a learning collaborative of organizations focused on improving the development and deployment of state-based all-payer claims databases (APCDs), supported by NAHDO members and other partners. (CHIA is a NAHDO member). The Learning Network calls are open to APCD programs and staff and meant to support APCD development through standardization and best practices, continuous improvement, and advocacy. Details and registration information will be available in the next NAHDO monthly newsletter; for more information, visit the NAHDO website.
CHIA is a member of NAHDO and participant in its events and annual conference. NAHDO’s next “Hot Topic webinar” will cover the future and importance of data standardization for March 11 at 3 p.m. EST. NAHDO also offers a monthly Data Quality Forum. For more information, and to subscribe to the NAHDO newsletter, visit the NAHDO website.
CENTER FOR HEALTH INFORMATION AND ANALYSIS
www.chiamass.gov